Two large national associations representing long-term care operators on Saturday emphasized the importance of communicating COVID-19 information to authorities and community residents and their family members as well as staff members.
Assisted living communities and skilled nursing facilities should notify their state survey agencies about residents and staff members who test positive for COVID-19, American Health Care Association / National Center for Assisted Living President and CEO Mark Parkinson said Saturday. AHCA / NCAL also encouraged providers to share the information with the Centers for Disease Control and Prevention, the Federal Emergency Management Agency and the Centers for Medicare and Medicaid Services.
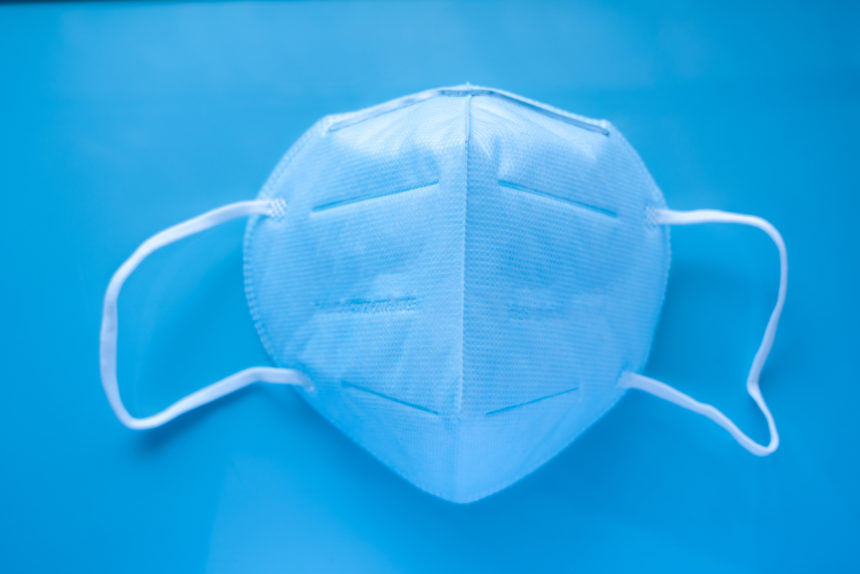
“We believe this information can help identify long-term care providers who are most in need of testing and [personal protective equipment] resources,” Parkinson said.
LeadingAge President and CEO Katie Smith Sloan issued a similar message. “We fully expect that consistent reporting of cases will lead to adequate and timely access to PPE and testing,” she said.
Additionally, AHCA / NCAL said, providers should notify all residents, families and staff members when a community has its first confirmed case of COVID-19.
Sloan made a similar recommendation. “Because COVID-19 impacts the people we serve, it is crucial that our members maintain transparent communication about positive cases with staff, residents and families,” she said. “Our members are on the front line caring for a vulnerable population.”
Operators ‘desperately need PPE’
Approximtely 90% of PPE in the national stockpile now has been distributed to state and local governments for them, in turn, to distribute how they determine is appropriate, according to a document released last week by the House Committee on Oversight and Reform. Senior living and care companies are looking elsewhere as well.
Operators “desperately need PPE,” AHCA / NCAL told McKnight’s Senior Living. “We are concerned about the nursing homes and assisted living communities that are exhausting their PPE supplies, and that is why we are calling for everyone to assist, including partners in other industries who may have PPE and the public, to do everything they can to assist us at this time,” the organization said.
The American Seniors Housing Association told McKnight’s Senior Living that lack of PPE and the “astronomical” increase in equipment costs have been “problematic” for operators across the country. “When Congress goes back and forms a commission to look at what went wrong with COVID-19, the inadequacy of PPE will surely be identified as a major problem along with the lack of testing capacity,” the organization said.
The CDC has a PPE burn rate calculator and optimization strategies on its website, Janine Finck-Boyle, LeadingAge vice president of regulatory affairs, told McKnight’s Senior Living.
“When you’re trying to make sure your staff have the equipment that’s needed, your residents have it, you’ll go through it pretty quickly,” she said. LeadingAge members, Finck-Boyle added, have been looking to multiple sources for PPE, especially masks.
Argentum said it continues to advocate for priority access to PPE for senior living operators. “This includes collaboration with our state partners and reaching out to governors (and by extension, state health commissioners), the U.S. Conference of Mayors, the National Association of Counties and the National Association of County and City Health Officials to share our concerns,” the association told McKnight’s Senior Living.
One state that prioritizes senior living
One state government that has prioritized senior living and skilled nursing for PPE is Arizona, Karen Barno, president and CEO of the Arizona Assisted Living Federation of America, told McKnight’s Senior Living. Arizona, according to azcentral.com, has received approximately 75% of its allocation from the national stockpile.
Gov. Doug Ducey (R) is “very pro-senior” and pro-veteran, Barno said, noting the state’s large senior population. Both groups, she said, were “pushed to the front of the line” for PPE.
“There are 35,000 beds in assisted living in Arizona,” Barno said. “That’s caring for a lot of seniors.”
Arizona ALFA, with assistance from Argentum, has been educating legislators and regulators about assisted living — “lobbying hard” — for the past couple of years, she said. “And then when we could see the pandemic taking place across the country and knowing that assisted living did not have a lot of PPE on hand at that moment, we knew we needed to hurry up and be able to receive PPE,” she said.
“We have a partnership with our nursing home association, LeadingAge and Arizona ALFA, which is one of the positive outcomes,” Barno added. “We’re all working as a team, putting our seniors first and how we care for our seniors, how can we make sure we have staffing for our seniors and more importantly, how do we protect our seniors, and that’s where the PPE comes in.”



